Students gather for in-person learning prior to the partial shutdown orders issued last week. (Photo from calvin.edu)
Students are getting sicker, ER visits increasing as COVID spike continues
Students with COVID-19 are currently exhibiting more serious symptoms than those who contracted the virus last fall and needing follow-up care from Health Services more frequently.
Emergency room visits averaged one to two per month during the fall semester. This semester, they’re averaging one to two per week, according to Sarah Visser, vice president for student life and co-chair of the COVID Response Team.
Two members of the Calvin community have been placed on ventilators in the ICU since the pandemic began and four students have spent time in the hospital due to COVID-related complications.
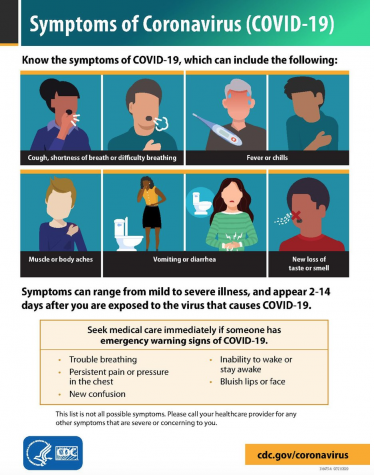
Freshman Madeline Scott contracted COVID on Friday, Feb. 5 but didn’t show symptoms until the following Sunday. Accustomed to getting migraines, Scott assumed the headaches and fatigue she experienced throughout the week were nothing to worry about. Then, on Feb. 12, she woke up with a fever and sore throat, unable to taste or smell. “My sore throat was so bad I couldn’t swallow or talk, and it was hard to breathe,” Scott told Chimes.
Scott’s parents advised her to go straight to the ER, where she tested positive for COVID-19.
“When they [the ER staff] found out I had COVID, they freaked out,” Scott said. “They were kind of scared to be around me.” After the ER visit, she reported her results to Health Services.
Scott has since made two more trips to the ER, both in response to recurring difficulties swallowing, talking and breathing. IVs for rehydration and pain medications were minimally effective at relieving her symptoms. “This is the first day I’ve felt good,” Scott said Tuesday.
Initial care for students who test positive on campus is provided through a virtual visit with a clinician who addresses any immediate symptoms. Clinicians then visit students in the dorms or allow them to come to the office for in-person appointments as necessary.
The five clinicians employed by Calvin (one part time, four full time) are currently meeting with 15-20 patients per day, five to six days per week. According to Visser, approximately 80% of these visits are COVID related.
Health Services personnel declined to comment on the increase in symptom severity.
“By comparison, last spring, summer, and fall, it was typical for 1 of those 15-20 daily cases seen by each provider to be experiencing more significant symptoms, such as high fevers, shortness of breath, chest pain, etc.” Visser said. “Over the past week or so, we have seen the number of patients experiencing more significant symptoms rise to nearly one-third of all patients.”
Residence life staff are contacting quarantined students once per week, and RAs are staying in touch with quarantined students on their floors. According to Becki Simpson, associate dean of residence life, “Our residence life professional staff are now calling every student who’s in quarantine to check in and see how they’re doing.”
Student case manager Kelsey Colburn is also available for students to contact about any resources they may need. “One thing I would like to impress upon students in Q&I,” Colburn said, “is that they shouldn’t hesitate to reach out to me if they have a question or concern. I can point them in the right direction and offer emotional support.”
Health Services provides pulse oximeters, peak flow meters and other respiratory monitoring devices to isolated students as needed. Clinicians also collaborate with local specialists to determine the best treatment for students who have underlying health conditions known to increase COVID risk.
“Patients with respiratory symptoms are assessed to determine if they need treatment measures beyond self-care or home-care treatment,” Visser said.
Clinicians are on the lookout for co-infections like influenza, mono and strep throat, but have not found them to be widespread on campus, Visser added.
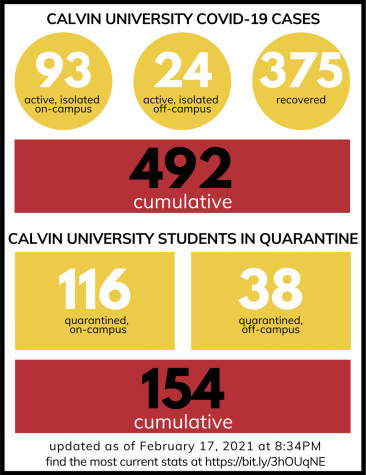
The COVID Response Team reported in a Feb. 16 email to the student body that there were currently 114 students in isolation and 206 students in quarantine.
“The tremendous burden [these numbers] put on our frontline workers is not sustainable,” the email stated, adding that any effects of recently increased distancing measures won’t be seen for 10 days or more.
“In the midst of this current case surge, our efforts are focused on providing timely care and assisting sick and worried students with getting the answers they need to care well for themselves,” Visser said.
A majority of students continue to report nothing more than minor symptoms and feel much better by the time they receive the results of their PCR tests, according to Visser.
The COVID Response Team is urging everyone to “stay the course” with masking and social distancing. Students can help slow the spread and protect themselves and others by following current lockdown guidelines and by reporting symptoms—even mild ones—promptly and accurately through the #CampusClear app and the Health Services patient portal.
“If you have a headache that’s not going away, there’s a good chance you have COVID,” Scott advised. “You should take my advice and actually do something about it.”
An earlier version of this article stated that two students were on ventilators. This article has been corrected to reflect that it was two members of the Calvin community, not two students. Chimes regrets the error.
