State of the Student: Health Services
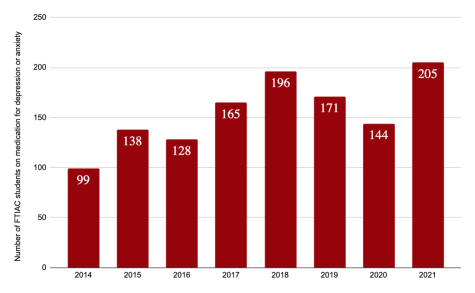
In 2015, depression and anxiety were the seventh most common reason for visits to Health Services. Just over 1,000 students visited for those reasons. In 2021, visits relating to depression and anxiety totalled almost 3,000, coming second only to COVID-19 in top reasons for visits. Over the same period, the number of incoming students reporting depression or anxiety medication at time of enrollment has increased from 138 to 205. Health Services’ primary care providers currently spend 40% of their time in the office providing mental health care. Fortunately, they are well equipped to do so.
Primary care providers provide most mental health care in the U.S., according to Health Services Director Laura Champion. “Depression and anxiety can be managed at a primary care office without any problem,” Champion told Chimes. Specialist psychiatrist support has notoriously long wait times with an average of 12 weeks. But Health Services’ partnership with Pine Rest brings two psychiatric physician’s assistants to campus one day a week, reducing the wait time for Calvin students to 3-10 days.
“In college health, if somebody’s needing more comprehensive care and the wait time is 2-4 months, that’s basically the rest of the semester. That’s not going to work,” Champion said. “Our goal has always been to find resources without as many obstacles.”
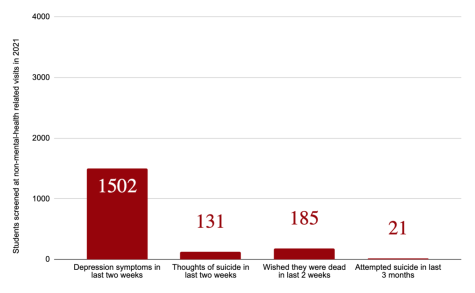
At 37% of non-mental health-related visits, students screened for depressive symptoms obtained positive scores. Nine percent of that group reported thinking of suicide in the past month, 12% reported thinking they wished they were dead in the past month and 1.4% reported an attempt to end their own life within the past three months.
Health Services uses a PHQ2 screening form, which measures depression symptoms over the past two weeks, on standard patients. A more detailed screening form is used for patients whose visit reason entails poor mental health symptoms. These tools are not diagnostic, Champion said. It’s the physician’s role to determine if the patient simply misunderstood the questions, there are extenuating circumstances, or if there is a mental health concern. In the latter case, “We change the direction of that appointment,” Champion said. If the patient has scored as moderate or high risk for suicide, the physician creates a Safety Plan with them at that same appointment.
In 2019, Health Service implemented a standard measurement systems for suicide risk. It’s now used across Health Services, the Center for Counseling and Wellness and Campus Safety, providing these different entities with what Champion calls “a shared language” for understanding suicide risk. Stanley-Brown Safety Plans were implemented for all moderate and high risk cases. These plans have been proven to help people experiencing mental health crises, Champion said. Six weeks after implementing the new system, COVID-19 hit. “It actually helped us much when we were trying to triage patients and they’re in isolation or they’re feeling down or they’re feeling lonely,” Champion said. “And so there’s a screening process to decide how to give them the right resources and how to figure out who’s in a crisis right now.” Health Services is “constantly trying to improve” at early intervention, according to Champion.
Health Services also serves as a link between students and on and off-campus resources. “We see ourselves as a portal to all sorts of support,” Champion said. “We see ourselves as an advocate to help get the right resources in place.”
Having a trained professional walking alongside you can make all the difference for students facing mental health struggles, according to Champion. Primary care providers at Health Services fill that need, either as sole provider or as a member of a care team.
Health Services has been able to keep up with demand for appointments, Champion said, but she noted that there are still “lots of students and friends of students who are hurting on campus who don’t know that Health Services is a resource.”